Not just helping us with road directions, finding favorite food joint, photo sharing and chat sessions, smart phones would soon diagnose diseases for us in real time.
Not just helping us with road directions, finding favorite food joint, photo sharing and chat sessions, smart phones would soon diagnose diseases for us in real time.
Researchers from University of Houston are developing a disease diagnostic system that offers results that could be read using only a smart phone and a Rs.1,200 lens attachment.
This new device relies on specific chemical interactions that form between something that causes a disease – a virus or bacteria, for example – and a molecule that bonds with that one thing only, like a disease-fighting antibody.
A bond that forms between a strep bacteria and an antibody that interacts only with strep, for instance, can support an iron-clad diagnosis.
“The trick is finding a way to detect these chemical interactions quickly, cheaply and easily. The device involves a simple glass slide and a thin film of gold with thousands of holes poked in it,” explained Jiming Bao, assistant professor of electrical and computer engineering at University of Houston.
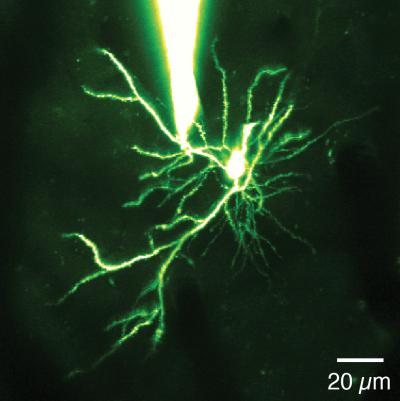
The device starts with a standard slide covered in a light-sensitive material known as a photoresist. It uses a laser to create a series of interference fringes – basically lines – on the slide, and then rotates it 90 degrees and creates another series of interference fringes.
The intersections of these two sets of lines creates a fishnet pattern of UV exposure on the photo-resist. The photo-resist is then developed and washed away.
While most of the slide is then cleared, the spots surrounded by intersecting laser lines – the ‘holes’ in the fishnet – remain covered, basically forming pillars of photo-resist.
The end result is a glass slide covered by a film of gold with ordered rows and columns of transparent holes where light can pass through. These holes are key to the system. The device diagnoses an illness by blocking the light with a disease-antibody bond – plus a few additional ingredients.
Here is where the smart phone comes in. “One of the advantages of this system is that the results can be read with simple tools,” said Richard Willson, Huffington-Woestemeyer professor of chemical and biomolecular engineering.
A basic microscope used in elementary school classrooms provides enough light and magnification to show whether the holes are blocked.
With a few small tweaks, a similar reading could almost certainly be made with a phone’s camera, flash and an attachable lens.
This system, then, promises readouts that are affordable and easy to interpret. There are some technical hurdles to clear before the system can be rolled out, Willson noted. One of the biggest challenges is finding a way to drive the bacteria and viruses in the sample down to the surface of the slide to ensure the most accurate results.
But if those problems are overcome, the system would be an excellent tool for health care providers in the field, said the research published in the journal ACS Photonics.