
In a feat that experts say is a significant advance for regenerative medicine, scientists have discovered a surprisingly simple method for creating personalized stem cells that doesn’t involve human embryos or tinkering with DNA.
Two studies published Wednesday in the journal Nature describe a novel procedure for “reprogramming” the blood cells of newborn mice by soaking the cells in a mildly acidic solution for 30 minutes. This near-fatal shock caused the cells to become pluripotent, or capable of growing into any type of cell in the body.
When the reprogrammed cells were tagged and injected into a developing mouse, they multiplied and grew into heart, bone, brain and other organs, the scientists found.
“It was really surprising to see that such a remarkable transformation could be triggered simply by stimuli from outside of the cell,” said lead study author Haruko Obokata, a biochemistry researcher at the RIKEN research institute in Japan. “Very surprising.”
The simplicity of the technique, which Obokata and her colleagues dubbed stimulus triggered acquisition of pluripotency, or STAP, caught many experts off-guard.
“So you mistreat cells under the right conditions and they assume a different state of differentiation? It’s remarkable,” said Rudolf Jaenisch, a pioneering stem cell researcher at MIT who was not involved in the study. “Let’s see whether it works in human cells, and there’s no reason why it shouldn’t.”
Obokata said that researchers had already begun experiments on human cells, but offered no details.
Due to their Zelig-like ability to form any number of specialized cells, pluripotent stem cells are considered the basic building blocks of biology. Scientists are working on ways to use them to repair severed spinal cords, replace diseased organs, and treat conditions as varied as diabetes, blindness and muscular dystrophy.
By using stem cells spawned from the patient’s own cells, replacement tissues would stand less of a chance of being attacked by the patient’s own immune system, researchers say. That would spare patients the need to undergo a lifetime regimen of dangerous, immune-suppressing drugs.
But progress toward these lofty goals has been slow, due in part to the challenges of current stem cell production methods. The practice of harvesting stem cells from human embryos makes many people uncomfortable, and some religious groups have pressed for limits or bans on their use. Even scientists who want to study them say they may not be practical for medical therapies because they could be rejected by a patient’s body.
Another approach is to rewind a patient’s own mature cells to a pluripotent state. Dr. Shinya Yamanaka, the first person to make these induced pluripotent stem cells, won a Nobel Prize for this work in 2012. However, the reprogramming process converts only about 1% of the cells into iPS cells, and questions remain about their long-term stability and safety.
The STAP method presents a simpler, cheaper and faster method of producing stem cells, said Chris Mason, a professor of regenerative medicine bioprocessing at University College London.
“How much easier can it possibly get,” Mason told the Science Media Centre, an English organization that promotes scientific understanding on controversial subjects.
“If it works in man, this could be the game changer that ultimately makes a wide range of cell therapies available using the patient’s own cells as starting material,” he said. “The age of personalized medicine would have finally arrived.”
The STAP approach was inspired by observations of plant cells that changed character when they were exposed to environmental stress, according to the research team from RIKEN and Harvard’s Brigham and Women’s Hospital in Boston.
Obokata and her colleagues set about “stressing” mouse blood cells in a variety of ways to see if they would change. They exposed them to heat, deprived them of nutrition and repeatedly poured them through narrow glass pipes.
The method they ultimately published involved placing the cells in an acid solution for 30 minutes and then spinning them in a centrifuge for five minutes. The process converted 7% to 9% of the original cells into STAP cells, Obokata said.
To see whether the cells had been reprogrammed, researchers engineered the mice with a gene that would cause their cells to glow a fluorescent green under ultraviolet light if they became pluripotent. After torturing the blood cells, they began to glow after three days and appeared to peak at seven days, suggesting that they had become pluripotent in just a week’s time. The researchers bolstered the cells’ ability to proliferate by treating them with hormones and an immune cell secretion called leukemia inhibitory factor.
To fully prove that they had become pluripotent, the STAP cells were injected into normal mouse embryos. The resulting offspring, called a chimera, were a mix of regular cells and glowing STAP cells.
Andrew McMahon, director of USC’s Eli and Edyth Broad Center for Regenerative Medicine, said the creation of a chimera was critical to proving that blood cells had changed in a fundamental way.
“That’s the most rigorous [test] you could possibly do,” said McMahon, who was not involved in the study. It shows that the STAP cells can make every type of cell in the embryo and that they “can organize in a normal-looking way, so that what comes out is a normal looking fetus.”
McMahon said the study was also surprising in that it showed that mature cells could be reprogrammed without having to divide.
“That’s why the change is so rapid, because the cells don’t have to undergo division for this to occur,” he said. “It’s a really interesting and novel finding.”
Yamanaka, who was not involved in the STAP study, said the research would undoubtedly help scientists understand the basic biology of cellular reprogramming.
“The findings are important,” said Yamanaka, who directs Kyoto University’s Center for iPS Cell Research.
The reasons why stress causes cells to drastically alter their function remains a mystery, Obokata and her colleagues said.
She declined to say whether the researchers were seeking a patent on the STAP procedure.
Source: latimes
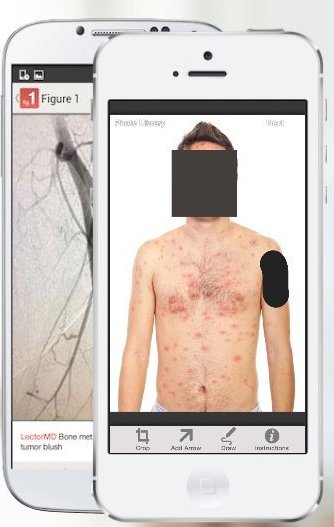 However, some experts have expressed concern about patient confidentiality. Patients’ faces are automatically obscured by the app but users must manually block identifying marks like tattoos.
However, some experts have expressed concern about patient confidentiality. Patients’ faces are automatically obscured by the app but users must manually block identifying marks like tattoos.




