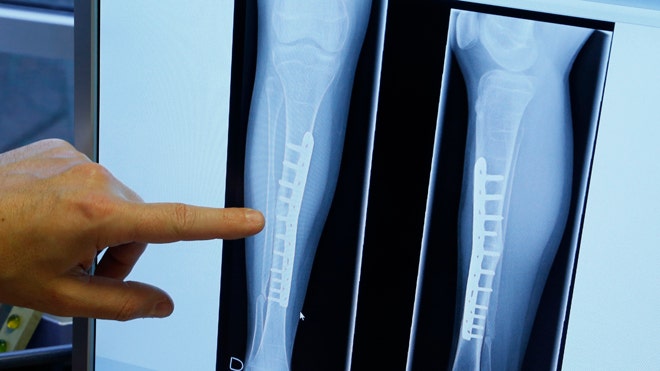
Screws made from 100% silk have been used to repair broken bones in research that could transform surgery.
US scientists say metal fixtures can potentially be replaced with plates and screws made from the natural fibre, which will eventually dissolve in the body.
So far the technique has only been tested on rodents. Silk was once used to make sutures, but more recently has been used in modern medical implants.
In the new research, a team of medical engineers at Tufts University, Massachusetts, made screws from medical grade silk using specially designed moulds. The silk material can be cut to different sizes on a machine.
The screws were implanted into the hind limbs of rats, where they functioned successfully for four to eight weeks.
By the end of the study, the silk had started to dissolve. The low stiffness of silk, which is similar to that of bone, and its ability to break down in the body, make it a promising bioengineering material compared with traditional metal plates and screws, the researchers say.
Lead researcher Dr David Kaplan said “The future is very exciting. We envision a whole set of orthopaedic devices for repair based on this – from plates and screws to almost any kind of device you can think of where you don’t want hardware left in the body.”
He added: “They don’t interfere with X-rays, they don’t set off alarms and they don’t cause sensitivity to cold.”
Recently, German researchers coated silicone breast implants with a thin layer of bioengineered silk proteins.
Preclinical studies suggest the coating reduces or prevents painful reactions.
The new research is published in the journal, Nature Communications.
Source: BBC news