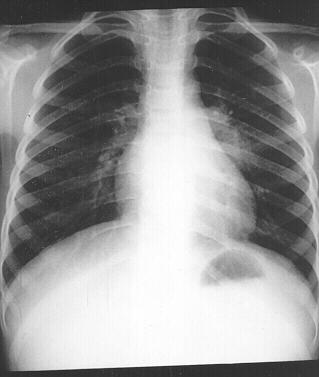
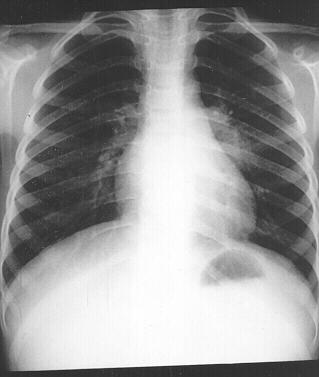
 Despite having a strong public sector programme to contain the disease, tuberculosis still remains a cause of concern for India, which has nearly a quarter of the global burden of TB, health experts said.
Despite having a strong public sector programme to contain the disease, tuberculosis still remains a cause of concern for India, which has nearly a quarter of the global burden of TB, health experts said.
Experts said measures which can help strengthen the fight against the disease include involvement of the private sector, more political commitment to create awareness and containing risk factors like malnutrition.
“TB is still a cause for concern. It is the sheer numbers in India and the associated problems like poverty which are responsible for this,” Soumya Swaminathan, director, National Institute for Research in Tuberculosis, an organization under the health ministry, told IANS.
According to the World Health Organization (WHO), there are 2.2 million tuberculosis patients in India, which makes it the world’s highest TB-burden country. TB killed 1.3 million people worldwide in 2012 and India alone accounted for 26 percent of the total cases.
She said that China and Brazil have done better in controlling TB in their respective countries and India needs to do more.
“In eight years, India has made tremendous progress as far as containing TB. But it needs to do much more,” she added.
But R. S. Gupta, deputy director general (TB) in the health and family welfare ministry, said: “Treatment success rates have been above 85 percent for several years in the country.”
Gupta told IANS that the overall quality of TB services, including human resources and systems for financial management are being strengthened.
To achieve the National Tuberculosis Programme’s (NTP) ambitious goal of universal health care access for all people with TB by 2017, financial commitments must be maintained by all partners, including international agencies, he said.
The state-run tuberculosis control initiative of the government, NTP provides free of cost, quality anti-tubercular drugs across the country. More than 1.5 million people avail the facility at 13,000 centres.
Gupta said that the private sector should be involved more as most patients are being treated in private clinics.
Agreed Swaminathan, who said that the government needs to work in tandem with the private sector.
“Standard procedures need to be followed for notification of the disease and diagnosis, especially by private practioners,” Swaminathan told IANS.
In 2012, India declared TB to be a notifiable disease. It means that with immediate effect all private doctors, caregivers and clinics treating a TB patient had to report every case to the government.
According to a recent WHO report, India has achieved the Millenium Development Goal (MDG) target for TB which says that the incidence of the disease should be falling. It is on track to reach the 2015 targets for reductions in TB prevalence and mortality.
But it added that India accounts for 31 percent of the estimated 2.9 million missed TB cases — people who were either not diagnosed or diagnosed but not reported to NTP.
It is estimated that about 40 percent of the Indian population is infected with TB bacteria, the vast majority of whom have latent rather than active TB.
Listing the other steps needed, Swaminathan said: “Getting more political commitment and activism from civil society to create awareness about TB like it was done in the case of HIV/AIDS would be a great help.”
India also needs to contain the risk factors associated with the disease. The biggest among them is malnutrition, which makes people more susceptible to the development of active TB. Tuberculosis patients have lower Body Mass Index (BMI), muscle mass and subcutaneous stores of fat.
“Malnutrition is the biggest risk factor and it has been overlooked,” she said, adding that the “disease needs to be fought on a common platform by all stakeholders.”
Source: Zee News


 Despite having a strong public sector programme to contain the disease, tuberculosis still remains a cause of concern for India, which has nearly a quarter of the global burden of TB, health experts said.
Despite having a strong public sector programme to contain the disease, tuberculosis still remains a cause of concern for India, which has nearly a quarter of the global burden of TB, health experts said.






