An app which enables healthcare professionals to share photos is to be rolled out across western Europe by the end of the year. The app was designed to enable doctors to share pictures of their patients, both with each other and with medical students.
So far, more than 150,000 doctors have uploaded case photos with the patient’s identity obscured. 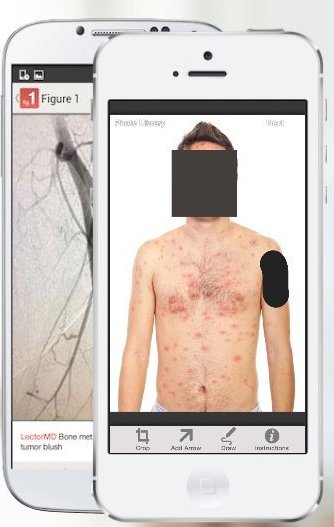 However, some experts have expressed concern about patient confidentiality. Patients’ faces are automatically obscured by the app but users must manually block identifying marks like tattoos.
However, some experts have expressed concern about patient confidentiality. Patients’ faces are automatically obscured by the app but users must manually block identifying marks like tattoos.
Each photo is reviewed by moderators before it is added to the database.
No secrets
Founder Dr Josh Landy told the BBC that the Figure 1 service did not access any patient records. “We do not possess any personal medical data at all. The best way to keep a secret is not to have it. We are not an organisation that delivers healthcare,” he told .
But doctors must provide identifying credentials and are also advised to notify their employees and patients to find out about consent policies. “Legally, we found that identifying the doctor does not identify the patient,” said Dr Landy.
“However some [medical] conditions are so rare that they can’t be posted. One user wanted to post something but there are only seven cases of it in the US and they had all been reportable because they are rare, so the patient could have been identified.” Anybody can download the app for free, but only verified healthcare professionals can upload photos or comment on them, he added.
‘Colourful’
“We reject sensationalistic images,” said Dr Landy. “Everything is there for educational purposes. That said, there are very colourful images – things medics see every day. It’s a transparent view into a world you rarely get to see.” The app is already available in North America, the UK and Ireland.
While digital services such as UpToDate and DynaMed – both requiring a subscription – are already widely used within the healthcare community as clinical knowledge databases, they are not rivals to Figure 1, said Dr Landy. “UpToDate is an app I love, and have used for years. However, they have a highly curated repository of articles written and edited by experts in the field.
“What our app does is provide the opportunity to contribute any case no matter how classic or unusual. Ours is all image-based and totally crowdsourced.” The app has received $6m (£3.75m) in investment in the last year. British GP and author Dr Ellie Cannon gave it a cautious welcome.
“I think it’s potentially really useful to share photos with medical students and other doctors,” she said. “Obviously the potential pitfall is the confidentiality. Of course, they are anonymised but even uploading from a certain doctor may go some way to identify a patient,” she added.
“And can a patient later opt out? We’ve seen with other sites the downsides of sharing too much.”
Source: bbc news