 Nevada’s university leaders have signed a partnership agreement to begin establishing a new M.D.-granting medical school in Southern Nevada.
Nevada’s university leaders have signed a partnership agreement to begin establishing a new M.D.-granting medical school in Southern Nevada.
The agreement, or memorandum of understanding, outlines a vision for UNLV and the University of Nevada School of Medicine at UNR to work together to create a four-year medical school at UNLV that would mint medical doctors.
The UNLV medical school would open under the University of Nevada medical school’s accreditation, but will eventually become its own independently operated, separately accredited and financially-sustainable medical school.
Nevada System of Higher Education Chancellor Dan Klaich, UNR President Marc Johnson, University of Nevada School of Medicine Dean Tom Schwenk and UNLV President Neal Smatresk signed the agreement on Wednesday. Nevada regents are expected to vote on the agreement at their December board meeting.
“Increasing the medical education and health care options for Nevadans has always been a top priority for the Nevada System of Higher Education,” Klaich said in a statement. “I’m proud of the collaboration between our two universities and their efforts to bring these long-discussed plans from the drawing board to reality.”
Earlier this year, Nevada’s higher education leaders — led by Regent Mark Doubrava — directed UNLV and UNR to begin developing plans for a UNLV medical school while continuing to develop the medical school at UNR. UNLV’s faculty senate and graduate student government also supported plans for an on-campus medical school.
Currently, UNR operates the University of Nevada School of Medicine; students complete their core classes in Reno and can complete their clinical training in Reno and at University Medical Center in Las Vegas.
Proponents of a UNLV medical school have long argued that the current model for medical education in Nevada has not served Southern Nevada, by solving its shortage of physicians. Las Vegas is the largest metropolitan area in the United States without an allopathic medical school.
Over the years, Nevada’s higher education leaders have proposed different ways to expand the current medical school’s footprint in Southern Nevada by purchasing a Las Vegas home for the medical dean and kicking around the idea for a $220 million academic medical center at UNLV.
Ultimately, regents decided upon creating a separate medical school for Southern Nevada that could educate high-quality physicians, spur new medical businesses and make Las Vegas a mecca for medical tourism.
“We’ve known for a long time that it is imperative that we build the health care capacity of Southern Nevada,” UNLV’s Smatresk said in a statement. “This collaborative agreement is a substantial step forward and offers a path that effectively utilizes the resources of two great institutions to address our critical needs in health care.”
The signed partnership agreement between UNR and UNLV would not only kickstart a second medical school in Nevada but help the two universities attract federal funding for medical research that would benefit northern, southern and rural communities.
“The ultimate goal is to best apply our resources and steward the investment placed in our organizations to result in improved medical care, health care services and quality of life for Nevadans,” UNR’s Johnson said in a statement.
Developing a Southern Nevada medical school will require a collaborative partnership not only between UNR and UNLV, but also among UMC, Las Vegas hospitals and the medical community. All parties must coordinate designing, financing and building a medical facility that will house clinical research and medical science training.
Building a Southern Nevada medical school will require “substantial incremental funding” from state and private sources, according to the partnership agreement. The construction cost for the UNLV medical school is expected to cost about $80 million.
The agreement calls for funding to be maintained to the UNR medical school and for more funding to create fellowships and residencies to keep physician interns in Nevada, where they are more likely to settle down and open a local practice.
“The quality of life and economic development of the state are dependent on our ability to educate more medical students, train more residents and fellows in more specialties and subspecialties, and improve the quality of care through clinical research,” Schwenk said in a statement. “This agreement is a huge step forward in accomplishing those goals.”
Earlier this year, UNLV’s Lincy Institute commissioned Tripp Umbach, a top national health care consulting firm, to conduct an economic impact study for a Southern Nevada medical school.
Tripp Umbach estimated that a UNLV School of Medicine could have a $1.9 billion total economic impact to Nevada, including the creation of 5,353 jobs and and $94 million in tax revenue by 2030. That represents six times the current economic impact of the UNR medical school, at $285 million.
The firm also recommended that UNLV medical school begin in 2016 with an initial class of 60 medical students, and grow to an incoming class of 120 students by 2030. To support its new medical school graduates and to retain them in-state, Tripp Umbach also advised that Las Vegas must create a minimum of 240 new residency positions.
In the coming months, higher education leaders will discuss the Tripp Umbach recommendations and set a timetable for the construction, programming, financing and accreditation of a UNLV medical school.
Source: Las vegas Sun











 Nevada’s university leaders have signed a partnership agreement to begin establishing a new M.D.-granting medical school in Southern Nevada.
Nevada’s university leaders have signed a partnership agreement to begin establishing a new M.D.-granting medical school in Southern Nevada.




 A man who suffered from a bloody cough that persisted for more than a year was surprised to find that the cause was a giant ball of fungus growing in his lung, according to a recent report of his case
A man who suffered from a bloody cough that persisted for more than a year was surprised to find that the cause was a giant ball of fungus growing in his lung, according to a recent report of his case

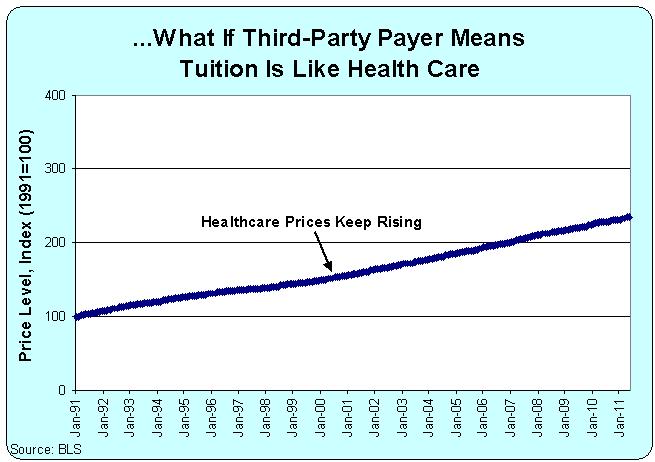 “In the case of medical education, students buy their education from medical schools and resell that education in the form of services to patients. Medical education can remain expensive only so long as there are patients, insurers, and employers who are willing to pay high prices for health care. But if prices for physician services decline, then the cost of medical education will have to decline too, or people won’t be willing to pay for medical school in the first place,” Asch says.
“In the case of medical education, students buy their education from medical schools and resell that education in the form of services to patients. Medical education can remain expensive only so long as there are patients, insurers, and employers who are willing to pay high prices for health care. But if prices for physician services decline, then the cost of medical education will have to decline too, or people won’t be willing to pay for medical school in the first place,” Asch says.