Patterns of “good” and “bad” cholesterol usually associated with heart risks also predicted the levels of Alzheimer’s-related beta amyloid protein seen in the brains of study participants.
“One of the important themes emerging from dementia research over the past 15 years is that there are intriguing connections between vascular disease and Alzheimer’s disease,” Bruce Reed, who led the research, told Reuters Health by email.
Reed is a professor and associate director of the University of California Davis Alzheimer’s Disease Research Center.
“It has become increasingly clear that what have been traditionally thought of as vascular risk factors – things like hypertension, diabetes and elevated cholesterol – are also risk factors for Alzheimer’s disease,” Reed said.
In previous work, Reed and his colleagues found a connection between overall vascular risk and levels of brain amyloid.
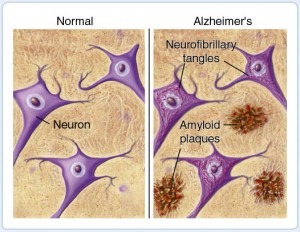
“Amyloid deposition is important because it is widely believed by scientists to be a key event that initiates a chain of events that eventually, years later, results in the dementia of Alzheimer’s disease,” Reed said.
“There was also previous work in cell cultures and with animals that suggested that cholesterol plays an important role in promoting the deposition of amyloid in the brain,” Reed said.
For the new study, published in JAMA Neurology, the researchers examined the cholesterol levels of 74 elderly people who had normal to mildly impaired cognitive function. Researchers also measured brain deposits of beta amyloid protein with positron emission tomography (PET scanning).
They found that on average, participants who had higher levels of the “bad” LDL cholesterol and lower levels of “good” HDL cholesterol also had higher levels of amyloid in the brain.
Elevated LDL-cholesterol is associated with cardiovascular disease while high levels of HDL-cholesterol are thought to protect against heart disease.
“We think this is a very important finding, but as with all novel findings it needs to be replicated,” Reed said. “Assuming that the basic pattern is found in other groups of patients, it is urgent that we try to understand the mechanism(s) behind this finding.”
“Cholesterol in blood and cholesterol in brain are separate ‘pools,’ walled off from one another by the blood brain barrier. We measured cholesterol in blood. So that is one question that needs to be answered – how do cholesterol levels in blood and in brain influence each other,” Reed said.
“And in the brain, it is not entirely understood how changing cholesterol levels might reduce amyloid deposition. We are very interested in the idea that higher HDL (‘good’) cholesterol levels may help the brain more efficiently clear the toxic amyloid at an early stage,” Reed said.
“If those questions were understood we could begin to think about how to change cholesterol levels so as to prevent the buildup of amyloid,” Reed added.
In other studies, some researchers have found evidence that LDL cholesterol-lowering drugs, such as statins, might offer some protection against Alzheimer’s disease, but the results have been inconsistent.
Reed’s team didn’t see any associations between current use of cholesterol medication by the participants and their amyloid levels.
In their report, Reed and his coauthors caution that the study does not prove cholesterol is directly affecting amyloid deposition. For instance, they write, unhealthy cholesterol could be linked to vascular damage, such as small strokes, and those micro-injuries could be the reason for the protein deposits.
He encourages people to follow the advice of their doctor and try to achieve the cholesterol guidelines set by the American Heart Association.
“A remarkable number of people who are alive now will live into their 80s or beyond – the period of highest risk for Alzheimer’s. This study is one more piece of evidence that what we do now can shape our health positively in those years,” Reed said.
Source: ABS CBN news

