IBM’s Watson supercomputer is being re-tasked to help clinicians create personalized treatments for a common form of brain cancer known as glioblastoma. The project, which is a collaboration between IBM and the New York Genome Center (NYGC), hopes to make use of Watson’s artificial intelligence to analyze vast quantities of data in order to suggest a personalized life-saving treatment based on the patient’s individual case.
Over the years, Watson has become faster and more compact. It differs from most ordinary computers in that, rather than simply observing patterns in data, Watson will actively learn and apply information to come to a reasoned hypothesis along with a level of confidence. Thus its cognitive process is more like that of a human being than a conventional computer. Furthermore, with the new Watson Discovery Advisor, the processing power and vast medical knowledge of Watson is accessible to clinicians via the cloud, allowing them to draw on the supercomputer’s analytical prowess from wherever they may be.
This is not the first time that Watson has been tasked with aiding in treatment for individuals suffering from cancer. The supercomputer was recently at work at the Memorial Sloan-Kettering Cancer Center where it aided and received tutelage from the staff, amassing an impressive medical database.
How will it work?
Watson’s general knowledge is about as comprehensive as it gets, having access to the entire volume of Wikipedia as well as a wealth of information from other sources. However, it is Watson’s ability to understand natural language and sift through vast quantities of case studies and articles, learning as it goes, that will be the key to allowing doctors to tailor patient specific treatments. IBM is hoping to utilize the NYGC’s expertise in the field of genomics to further develop and streamline Watson’s cognitive reasoning in the field of oncology.
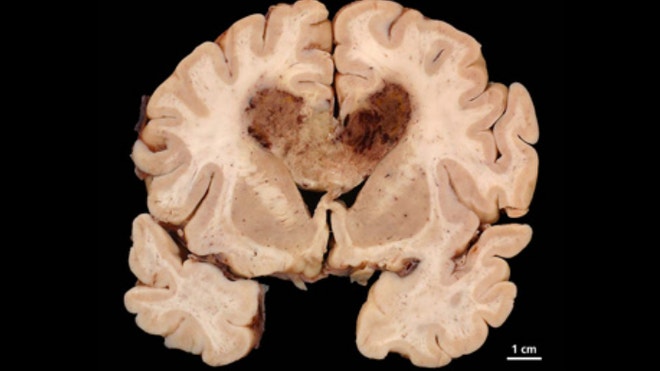
Watson will interpret genomic data from a set of patients diagnosed with glioblastoma, an aggressive form of brain cancer responsible for the deaths of around 13,000 Americans each year. The cloud-based prototype will attempt to expose the underlying genetic characteristics of this malignant cancer, using a combination of modern genomic analytics and its extensive bio-medical literature database.
Dr. Robert Darnell, CEO, President and Scientific Director of the NYGC, stated regarding the difficulties of targeted treatment that “The real challenge has been making sense of massive quantities of genetic data and translating research findings into better treatments and outcomes for patients.”
This is where Watson excels, applying its substantial computing power to observe gene sequence variations between ordinary and cancerous tumors. It consults clinical records and medical literature as it does so, swiftly giving doctors a variety of treatments to choose from, tailored to the patient’s individual instance of cancer.
Watson’s ability to achieve this task at a much higher speed than is otherwise possible, will prove to be greatly beneficial to those suffering from glioblastoma, as the general prognosis (depending on the spread of the cancer) is often less than one year. Ordinarily a significant portion of this time is spent interpreting the data manually to divine the best course of treatment. However, with Watson’s computing power, this can be achieved in a fraction of the time, allowing clinicians to begin life-saving treatment much sooner.
Dr. John E. Kelly, Senior Vice President and Director of IBM Research, believes that application of the cloud-based system will eventually extend beyond the targeted treatment of glioblastoma, stating that “With this knowledge, doctors will be able to attack cancer and other devastating diseases with treatments that are tailored to the patient’s and disease’s own DNA profiles. This is a major transformation that can help improve the lives of millions of patients around the world.”
The following video outlines how Watson will seek to streamline the current treatment process.
source: gizmag