The Nobel Assembly at Karolinska Institutet on Monday decided to award the 2014 Nobel Prize in Physiology or Medicine with one half to John O´Keefe and the other half jointly to May-Britt Moser and Edvard I Moser for their discoveries of cells that constitute a positioning system in the brain.

ohn O’Keefe was born in 1939 in New York, US. He is currently affiliated with the University College, London, UK. May-Britt Moser was born in 1963 in Fosnavag, Norway. She is currently affiliated with the Centre for Neural Computation, Trondheim, Norway. Edvard I Moser was born in 1962 in Alesund, Norway. He is currently affiliated with the Kavli Institute for Systems Neuroscience, Trondheim, Norway.
How do we know where we are? How can we find the way from one place to another? And how can we store this information in such a way that we can immediately find the way the next time we trace the same path? This year´s Nobel Laureates have discovered a positioning system, an “inner GPS” in the brain that makes it possible to orient ourselves in space, demonstrating a cellular basis for higher cognitive function.
In 1971, John O´Keefe discovered the first component of this positioning system. He found that a type of nerve cell in an area of the brain called the hippocampus that was always activated when a rat was at a certain place in a room. Other nerve cells were activated when the rat was at other places. O´Keefe concluded that these “place cells” formed a map of the room.
More than three decades later, in 2005, May-Britt and Edvard Moser discovered another key component of the brain’s positioning system. They identified another type of nerve cell, which they called “grid cells”, that generate a coordinate system and allow for precise positioning and pathfinding. Their subsequent research showed how place and grid cells make it possible to determine position and to navigate.
The discoveries of John O´Keefe, May-Britt Moser and Edvard Moser have solved a problem that has occupied philosophers and scientists for centuries – how does the brain create a map of the space surrounding us and how can we navigate our way through a complex environment?
How do we experience our environment?
The sense of place and the ability to navigate are fundamental to our existence. The sense of place gives a perception of position in the environment. During navigation, it is interlinked with a sense of distance that is based on motion and knowledge of previous positions.
Questions about place and navigation have engaged philosophers and scientists for a long time. More than 200 years ago, the German philosopher Immanuel Kant argued that some mental abilities exist as a priori knowledge, independent of experience. He considered the concept of space as an inbuilt principle of the mind, one through which the world is and must be perceived. With the advent of behavioural psychology in the mid-20th century, these questions could be addressed experimentally. When Edward Tolman examined rats moving through labyrinths, he found that they could learn how to navigate, and proposed that a “cognitive map” formed in the brain allowed them to find their way. But questions still lingered – how would such a map be represented in the brain?
John O´Keefe and the place in space
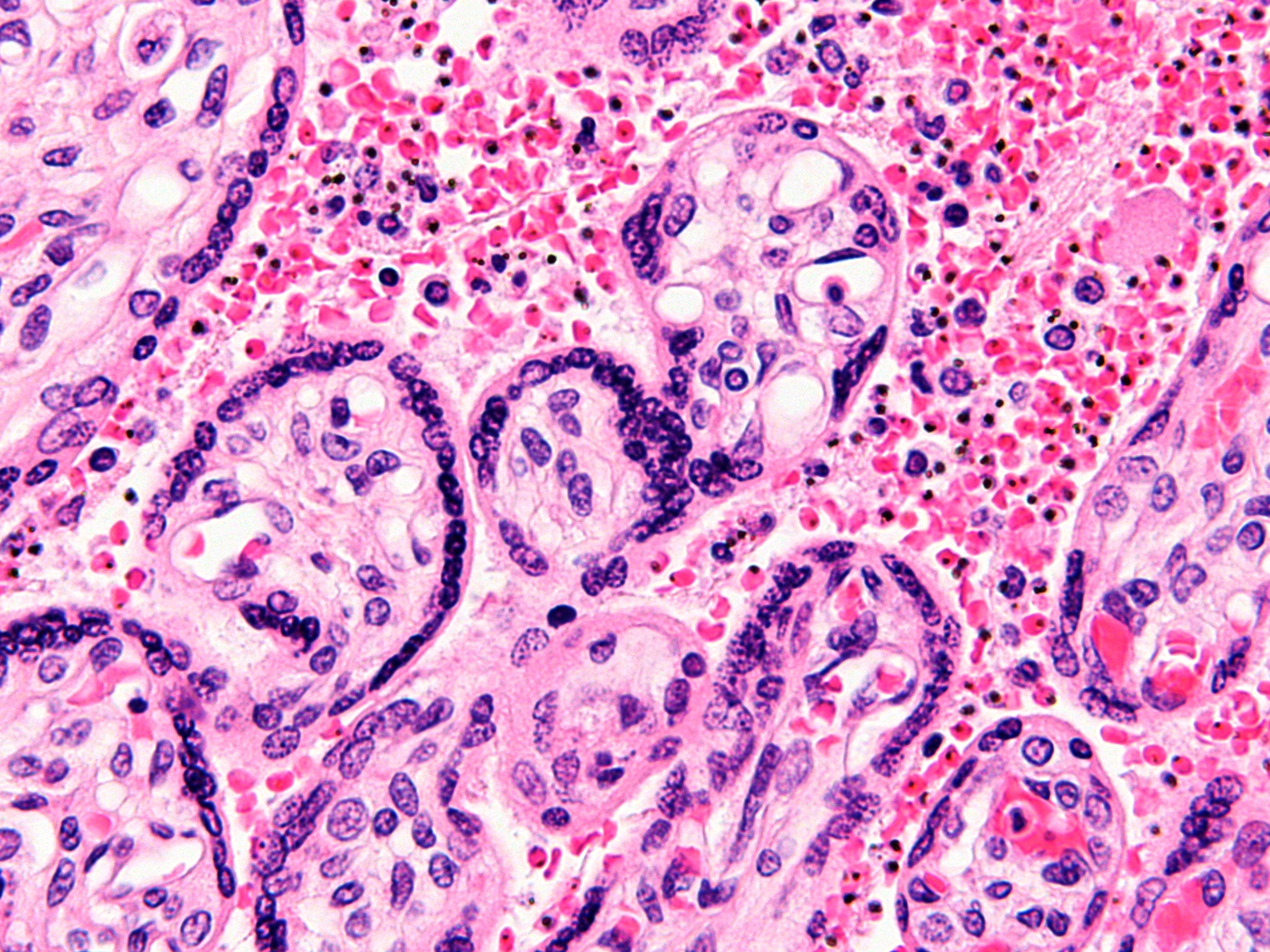
John O´Keefe was fascinated by the problem of how the brain controls behaviour and decided, in the late 1960s, to attack this question with neurophysiological methods. When recording signals from individual nerve cells in a part of the brain called the hippocampus, in rats moving freely in a room, O’Keefe discovered that certain nerve cells were activated when the animal assumed a particular place in the environment (Figure 1). He could demonstrate that these “place cells” were not merely registering visual input, but were building up an inner map of the environment. O’Keefe concluded that the hippocampus generates numerous maps, represented by the collective activity of place cells that are activated in different environments. Therefore, the memory of an environment can be stored as a specific combination of place cell activities in the hippocampus.
May-Britt and Edvard Moser find the coordinates
May-Britt and Edvard Moser were mapping the connections to the hippocampus in rats moving in a room when they discovered an astonishing pattern of activity in a nearby part of the brain called the entorhinal cortex. Here, certain cells were activated when the rat passed multiple locations arranged in a hexagonal grid (Figure 2). Each of these cells was activated in a unique spatial pattern and collectively these “grid cells” constitute a coordinate system that allows for spatial navigation. Together with other cells of the entorhinal cortex that recognize the direction of the head and the border of the room, they form circuits with the place cells in the hippocampus. This circuitry constitutes a comprehensive positioning system, an inner GPS, in the brain (Figure 3).
A place for maps in the human brain
Recent investigations with brain imaging techniques, as well as studies of patients undergoing neurosurgery, have provided evidence that place and grid cells exist also in humans. In patients with Alzheimer´s disease, the hippocampus and entorhinal cortex are frequently affected at an early stage, and these individuals often lose their way and cannot recognize the environment. Knowledge about the brain´s positioning system may, therefore, help us understand the mechanism underpinning the devastating spatial memory loss that affects people with this disease.
The discovery of the brain’s positioning system represents a paradigm shift in our understanding of how ensembles of specialized cells work together to execute higher cognitive functions. It has opened new avenues for understanding other cognitive processes, such as memory, thinking and planning.
Source: india medical times