An experimental therapy for a blinding eye disease showed early – and surprising – promise when it improved the vision of patients in an early trial that was only supposed to test its safety, doctors reported Wednesday.
The experimental gene therapy not only stopped the steady degeneration of the patients’ vision, but appears to have reversed some of the damage. And the effects have lasted two years in one case, British researchers report in the Lancet medical journal.
Wayne Thompson of Staffordshire in Britain saw the stars for the first time in years after being treated in April.
“One night in the summer, my wife called me outside as it was a particularly starry evening. As I looked up, I was amazed that I was able to see a few stars,” Thompson, 43, said in a statement.
“I hadn’t seen stars for a long, long time,” he added.
“It is still too early to know if the gene therapy treatment will last indefinitely, but we can say that the vision improvements have been maintained for as long as we have been following up the patients, which is two years in one case,” says Dr. Robert MacLaren of the Nuffield Laboratory of Ophthalmology at the University of Oxford, who leads the research team.
“In truth, we did not expect to see such dramatic improvements in visual acuity and so we contacted both patients’ home opticians to get current and historical data on their vision in former years, long before the gene therapy trial started. These readings confirmed exactly what we had seen,” he added in a statement.
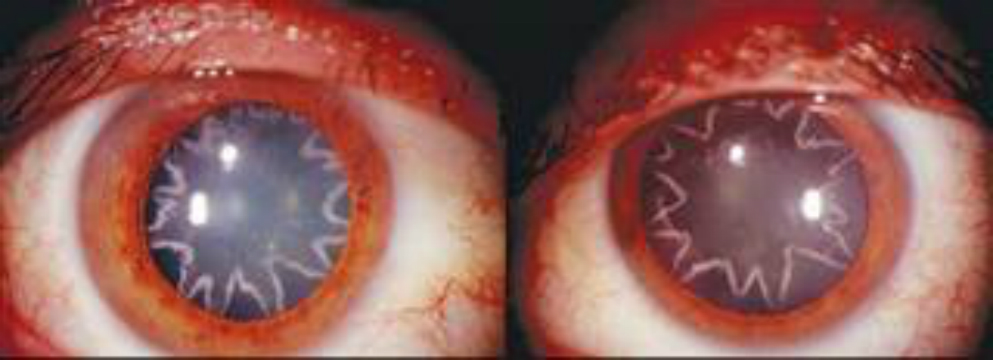
The men taking part in the trial all have choroideremia, a genetic disease that causes vision to start breaking down when patients are still children. The defective gene, called CHM, is on the x chromosome, so it almost exclusively affects males – females have an extra x chromosome that usually makes up for any lost function. It causes about 4 percent of all cases of blindness, according to the National Institutes of Health.
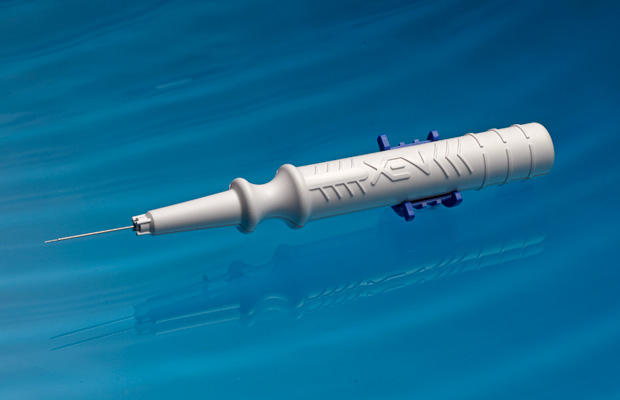
The condition breaks down various parts of the retina, the reflective tissue at the back of the eye that collects light and images. The gene therapy approach uses a virus to carry a corrective gene directly into the retina.
Gene therapy itself has a mixed record – it’s harder than scientists thought to safely deliver new genes into the body. And there is no guarantee that the patient’s cells will accept the new gene and use it.
But the eye is a good place to try, in part because doctors can see the effects in real time, and also because one eye can be treated and the other eye used to compare results.
“I think that this is a very important study,” said Dr. Richard Weleber, professor of ophthalmology who is leading a team at Oregon Health and Science University trying gene therapy to treat Usher Syndrome.
MacLaren’s trial was meant to be a stage 1 safety trial, designed simply to show that the treatment did no harm. But the six patients in the trial said they noticed improvements quickly.
“This has huge implications for anyone with a genetic retinal disease such as age-related macular degeneration or retinitis pigmentosa, because it has for the first time shown that gene therapy can be applied safely before the onset of vision loss,” MacLaren said.
He says nine patients have now had one eye treated with the gene therapy in operations at the Oxford Eye Hospital. The patients had varying degrees of vision loss, but MacLaren thinks the best course will be to treat people when they are young, before much damage has been done.
“If we were able to treat people early, get them in their teens or late childhood, we’d be getting the virus in before their vision is lost,” he said. “If the treatment works, we would be able to prevent them from going blind.”
Weleber, who says his own gene therapy trial is moving along but who could not release details, says MaCLaren’s surgical technique may have helped the therapy work more successfully. MacLaren’s team lifted an area called the macula to deliver the engineered viruses directly into the tissue that needed correcting.
Last year, researchers reported success against a different genetic disease causing blindness , one called Leber congenital amaurosis. But even though the patients’ vision improved, the eye continued to deteriorate.
“Each type (of genetic disease) needs to be tested separately,” Weleber said.
Gene therapy also works to some degree against blood cancers and immune diseases.
Last year, doctors reported they had successfully treated the first children in the U.S. for severe combined immune deficiency or SCID, sometimes known as “bubble boy” disease. Like choroideremia, SCID is caused by a mutated recessive gene, meaning children must inherit a defective copy from each parent to show symptoms.
Gene therapy has helped 26 of 59 two patients with a form of cancer called chronic lymphocytic leukemia go into remission after a type of gene therapy treatment that programmed immune system cells to hunt down and kill the leukemia cells. And last year doctors reported 24 people with acute lymphocytic leukemia got at least temporary remission after gene therapy.
Source: nbc news