
Brain cells of patients with bipolar disorder act differently than those of people without the mental illness, according to scientists who conducted a stem cell study of the condition.
The investigators said their research might one day lead to a better understanding of bipolar disorder and new treatments for the disease, which causes extreme emotional highs and lows.
About 200 million people worldwide have bipolar disorder. “We’re very excited about these findings. But we’re only just beginning to understand what we can do with these cells to help answer the many unanswered questions in bipolar disorder’s origins and treatment,” said study co-leader
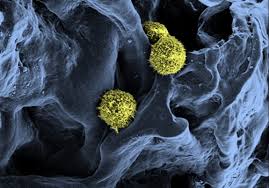
Dr. Melvin McInnis, a professor of bipolar disorder and depression at the University of Michigan Medical School. The study authors took skin stem cells from people with and without bipolar disorder and transformed them into neurons similar to brain cells. It’s the first time that stem cell lines specific to bipolar disorder have been created, the researchers said.
They discovered distinct differences in how the two sets of neurons behave and communicate with each other. The cells also differed in their response to lithium, the most widely used treatment for bipolar disorder.
The study was published online March 25 in the journal Translational Psychiatry.
“This gives us a model that we can use to examine how cells behave as they develop into neurons,” study co-leader Sue O’Shea, a professor in the department of cell and developmental biology and director of the University of
Michigan Pluripotent Stem Cell Research Lab, said in a university news release.
“Already, we see that cells from people with bipolar disorder are different in how often they express certain genes, how they differentiate into neurons, how they communicate, and how they respond to lithium,” O’Shea said.
McInnis said it’s possible the research could lead to new types of drug trials. If it becomes possible to test new drug candidates in these cells, patients would be spared the current trial-and-error approach that leaves many with uncontrolled symptoms, he said.
Source: News max health








 Australian scientists have developed a hi-tech handheld ‘biopen’ that can enable surgeons to draw new bone material onto seriously injured people.
Australian scientists have developed a hi-tech handheld ‘biopen’ that can enable surgeons to draw new bone material onto seriously injured people.