Union Health Minister Dr Harsh Vardhan has said that he would request the Ministry of Human Resource Development to include in school text books passages and essays that generate in young children a positive attitude towards organ donation in general and eye (cornea) donation in particular.
The minister, who was speaking at the centenary celebrations of Shroff’s Charity Eye Hospital in Delhi on Saturday, stated that the ongoing National Eye Donation Fortnight (August 25 – September 8), an annual event organised by the National Programme for Control of Blindness, is meeting with good response in a large number of states, including Delhi. It is now felt that youngsters should be exposed to the enormity of the problem of blindness in India and their responsibility to contribute to its end.
“We teach the young the life stories of great savants and leaders with the hope that the new generation will imbibe their qualities. It is also necessary to instil in them their responsibility towards the blind population of India which could benefit if cornea donation becomes part of the nation’s culture,” Dr Harsh Vardhan said.
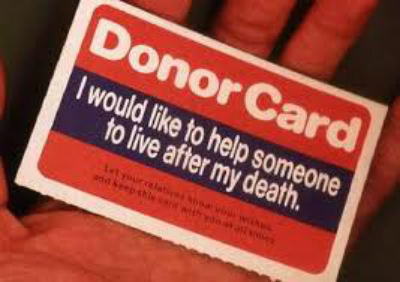
He said that eyesight is one of the biggest gifts of God. Unfortunately, the corneal blind population of India is the largest in the world. At a rough estimate, the country needs 1 lakh corneas every year but only about 17,000 are procured. Of these only about 50 per cent are utilised.
According to WHO, there are 45 million blind persons in the world, of whom 12 million are in India. Corneal blindness accounts for 1 per cent of the total blind population of the country. WHO also estimates that the blind population may double by 2020 owing to the rise in population and longevity.
The minister observed, “We need more eye banks. But that is not enough. There should be synergistic interaction among professional health services and community engagement. Increasing public awareness, promoting eye donation, implementing quality standards and organising a network of trained professionals for procurement, preservation and distribution of tissues are vital cogs in the wheel.”
Dr Harsh Vardhan said the history of ophthalmology in the country is inextricably linked to the vision of Dr S P Shroff, who founded the institution in 1914. “Dr S P Shroff was a founding father of the Delhi Medical Association, the precursor of the Indian Medical Association. Both Shroff’s hospital and DMA were established in the same year and have proved to be lasting institutions that have contributed much to India’s development,” he remarked.
The tradition of pledging one’s eyes after death is quite old in Delhi thanks to the pioneering work by Shroff’s Hospital, the minister said. At the function, a number of facilitators and donors’ families from Delhi, Karnal and other places of northern India were honoured, including the parents of a 14-year-old girl and the son of a 65-year-old man. In both cases, the family members showed exemplary presence of mind while making the emotionally heavy choice of donating the just-deceased’s eyes.
In this context, Dr Harsh Vardhan recalled the case of Surabhi, the 16-year-old girl from Krishna Nagar, Delhi, who was declared brain dead in 2013 after being admitted to AIIMS. Her parents took the tough decision to donate her organs for the benefit of people who needed her cornea, heart, liver and other body tissues.
Dr Harsh Vardhan said that within a month, the web portal of the National Organ and Tissue Transplant Organisation (NOTTO) will become functional. With that it would be possible to establish a transparent interface between donors and recipients of all organs including cornea.
The government intends implementing a nationwide programme for setting up regional centres modelled on NOTTO at Chandigarh, Guwahati, Kolkata, Chennai and Mumbai. All the upcoming AIIMS at six cities will also have similar infrastructure.
Dr Noshir M Shroff, medical director of Shroff Eye Centre; Dr Madan Mohan, a reputed ophthalmologist; Dr Sara Varughese, a senior ophthalmologist who heads the “Vision 2020” organization; Dr Umang Mathur, medical director of Shroff’s Charity Eye Hospital; and A K Arora, administrator of Shroff’s Eye Charity Hospital, were present on the occasion.
Source: IMT