The first patient fitted with an artificial heart made by the French company Carmat has died, the hospital that had performed the transplant in December said on Monday.
The 76-year-old man died on Sunday, 75 days after the operation, the Georges Pompidou European Hospital in Paris said in a statement, adding that the cause of his death could not be known for sure at this stage.
When he was fitted with the device, the man was suffering from terminal heart failure, when the sick heart can no longer pump enough blood to sustain the body, and was said to have only a few weeks, or even days, to live.
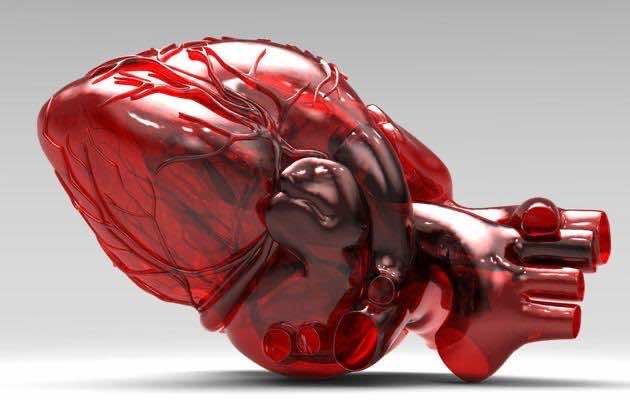
Carmat’s bioprosthetic device is designed to replace the real heart for as much as five years, mimicking nature’s work using biological materials and sensors. It aims to help the thousands of patients who die each year while awaiting a donor, and reducing the side-effects associated with transplants.
“Carmat wishes to pay tribute to the courage and the pioneering role of this patient and his family, as well as the medical team’s dedication,” a company spokeswoman said.
She stressed that it was premature to draw any conclusions on Carmat’s artificial heart at this stage.
Three more patients in France with terminal heart failure are due to be fitted with the device. The clinical trial will be considered a success if the patients survive with the implant for at least a month.
If it passes the test, Carmat has said it would fit the device into about 20 patients with less severe heart failure.
EXTENDING LIFE
“The doctors directly involved in the post-surgical care wish to highlight the value of the lessons learned from this first clinical trial, with regard to the selection of the patient, his surveillance, the prevention and treatment of difficulties encountered,” the hospital said in its statement.
An in-depth analysis of the medical and technical data gathered since the patient’s operation will be needed to establish the cause of his death, the hospital added.
Carmat estimates around 100,000 patients in the United States and Europe could benefit from its artificial heart, a market worth more than 16 billion euros ($22 billion).
Among Carmat’s competitors for artificial heart implants are privately-held SynCardia Systems and Abiomed, both of the United States.
SynCardia’s artificial heart is the only one approved both in the United States and the European Union and has been implanted in more than 1,200 patients to keep them waiting for a heart from a matching donor. The longest a patient has lived with the device is just under four years prior to a transplant.
Carmat’s heart is designed to serve not as a bridge to transplant but as a permanent implant, extending life for terminally ill patients who cannot hope for a real organ, generally because they are too old and donors too scarce.
Source: Reuters